Health
A Look at the Complex Causes and Symptoms of Nasopharyngeal Carcinoma
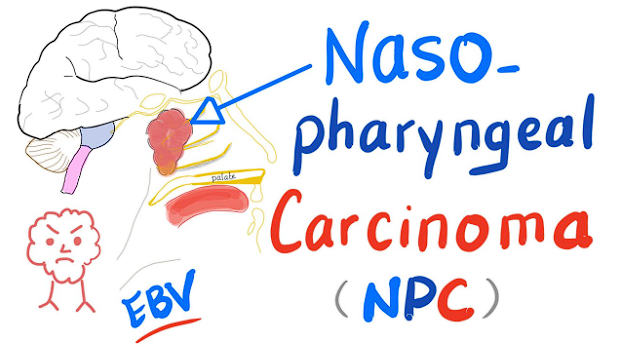
Nasopharyngeal carcinoma (NPC) is a type of cancer that occurs in the nasopharynx, which is located at the back of the nose and the top part of the throat. It can be difficult to detect NPC in its early stages, but some common symptoms may indicate a problem. In this article, we will discuss some of the most common symptoms associated with nasopharyngeal carcinoma. We will also discuss how to recognize these signs and when to seek medical attention for them.
Nasopharyngeal carcinoma symptoms may include a lump in the neck, enlarged lymph nodes, headaches, ear pain and hearing loss, facial pain or numbness, difficulty swallowing and speaking, bleeding from the nose or coughing up blood.
The cause of NPC is unknown but some factors are believed to increase risk such as smoking cigarettes or being exposed to certain chemicals found in paints and solvents. Other risk factors include Epstein-Barr virus infection (EBV), family history of NPC as well as people with certain genetic mutations like Fanconi anaemia.
Diagnosis of NPC involves having imaging tests such as CT scans or MRI scans done on your neck area to look for any abnormalities that could potentially be cancerous tissue.
Causes
Nasopharyngeal carcinoma is a rare cancer that affects the nasopharynx, which is the area at the back of your nose and near your throat. It can be difficult to detect because it often does not cause any symptoms in its early stages. Although the exact cause of this type of cancer is unknown, several factors have been identified that may increase a person’s risk of developing it.

The Epstein-Barr virus (EBV) has been linked to nasopharyngeal carcinoma. This virus is very common and most people who have it do not develop this type of cancer. However, people with an active EBV infection are more likely to develop nasopharyngeal carcinoma than those without an active infection. Smoking cigarettes also increases a person’s risk of developing this type of cancer as well as other types of head and neck cancers. People who smoke heavily or for a long period are more likely to develop these cancers than those who don’t smoke at all or only occasionally smoke cigarettes.
One potential symptom of Nasopharyngeal Carcinoma is earaches or ear pain. This type of pain might come and go or become more severe over time. It might also radiate into the temple area or cause hearing loss if left untreated.
Swollen neck glands or lymph nodes may also appear in people with NPC. These nasopharyngeal carcinoma symptoms typically located near the ears, jawline, and behind the collarbone and may feel tender when touched. Swelling could also occur in other areas of the head and neck due to metastatic disease spreading from primary tumour sites elsewhere in the body such as the lungs, liver etc.
Diagnosis and Treatment
Nasopharyngeal carcinoma is a rare cancer that forms in the nasopharynx, which is the upper part of the throat behind the nose. It is often linked to certain viruses and can spread to nearby lymph nodes and other parts of the body. Diagnosis and treatment options for this type of cancer vary depending on how advanced it is.
Diagnosis for nasopharyngeal carcinoma usually begins with a physical exam, during which your doctor will check for swollen lymph nodes or any other signs of abnormal tissue growth. Imaging tests such as computed tomography (CT) scans or magnetic resonance imaging (MRI) may be used to get a better look at possible tumours or abnormal tissue growths in your throat or neck area. A biopsy may also be done if an area looks suspicious enough to warrant further investigation.
Treatment options depend on how advanced your cancer is when it’s diagnosed, as well as its size and location. Surgery may be recommended to remove tumours from hard-to-reach areas, while radiation therapy may be used in combination with chemotherapy drugs to target larger areas affected by cancer cells.
Conclusion
Nasopharyngeal carcinoma symptoms can vary greatly from person to person and may include nasal congestion, earache, hearing loss, persistent sore throat, neck pain or lumps, facial swelling and difficulty swallowing. Early diagnosis is key as treatment options are more effective when the cancer is found in its early stages. If you experience any of these symptoms it is important to get a medical evaluation as soon as possible.
Health
Signs It is Time to Consider Dementia Care for an Aging Loved One

Life changes for everyone as age advances, and so do the needs that come with it. Families may start noticing subtle shifts in a loved one’s behavior, memory, or independence. These changes can be confusing, and understanding when additional support becomes necessary can feel difficult. The goal is always to ensure comfort, safety, and dignity; values that matter most when caring for someone close to your heart.
When memory loss and confusion begin disrupting daily life, families look for trusted support. Dementia care becomes a meaningful path to maintaining a loved one’s quality of life while reducing emotional strain on family members. Recognizing the right time to take that step can help create stability and peace for everyone involved.
Increased Forgetfulness Beyond Normal Aging
Memory lapses can appear harmless at first. Forgetting appointments or names occasionally happens to many people. But when these incidents become persistent or increasingly severe, they may signal something more than ordinary aging. You might notice your loved one misplacing items in unusual spots, repeating the same questions within minutes, or struggling to recall familiar faces. What stands out is the disruption these moments create. A decline that affects day-to-day tasks or causes distress can signal a deeper cognitive issue. This is when professional support can provide the structured attention and safety your loved one truly needs.
Noticeable Changes in Behavior and Personality
Behavioral changes usually emerge early and can feel unexpected. A previously social individual may become withdrawn or irritable without a clear reason. Some begin expressing suspicion toward relatives or show mood swings that seem unrelated to circumstances. Such shifts can create emotional tension within families and raise concerns about well-being. Because emotional stability is closely tied to safety, increasing agitation or a decline in judgment calls for more attentive supervision. Compassionate care under the guidance of dementia-trained professionals can help manage these challenges while preserving the individual’s sense of comfort and respect.
Difficulty Managing Daily Routines
Everyday activities form the foundation of independence. When a loved one starts struggling with basic routines such as preparing meals, dressing appropriately, or taking medications, it becomes a red flag. Missed meals, unwashed laundry, or neglected hygiene indicate that assistance is now necessary. Loss of routine can make schedules chaotic and environments unsafe. Balancing family responsibilities with constant supervision is stressful, leading many families to explore dementia care options that provide consistent, reliable structure. Professional assistance ensures regularity and safeguards health while easing family pressures.
Decline in Communication and Decision-Making
Clear expression is crucial for connection and confidence. As cognitive abilities decline, finding words or following conversations becomes harder for many older adults. Simple discussions may leave them frustrated or silent. Some might also lose the ability to make sound decisions about finances or personal safety. Loved ones struggle to interpret their needs, creating friction and emotional strain. Professional care designed for memory support helps bridge this gap. Trained caregivers encourage positive interaction, using compassionate approaches that restore dignity and reduce moments of confusion.
Wandering or Getting Lost in Familiar Places
Fear grows quickly when a family member goes missing unexpectedly. Wandering behavior is one of the strongest indicators that specialized help is essential. Someone who once walked confidently to the local shop might suddenly lose their way home. The sense of direction or memory of surroundings diminishes, leading to real danger. In such cases, immediate intervention can prevent accidents or distress. Secure supervision through structured care can protect your loved one without compromising their sense of freedom. Preventive attention ensures safety, reassurance, and peace of mind for families.
Increased Dependence and Physical Safety Concerns
Physical safety becomes a central concern with cognitive decline. Slower responses and reduced awareness raise the risk of falls, burns, or mishandling household equipment. Family members might start observing bruises, broken items, or neglected living spaces. These signs signal the need for professional oversight. In environments designed for people with memory impairments, safety measures exist at every level. From fall prevention to meal assistance, specialized caregivers ensure security while fostering confidence. This support reduces family anxiety and enhances your loved one’s daily experience.
Growing Stress on Family Caregivers
Caring for an aging parent or spouse demands patience, energy, and emotional strength. Families reach a point where the balance between caregiving and personal life becomes unmanageable. Persistent exhaustion, burnout, or guilt appear as warning signs that help is overdue. Recognizing those limits does not mean giving up. It reflects a deep commitment to a loved one’s comfort and happiness. Professional support brings relief from constant worry and allows family members to reclaim moments of connection rather than stress.
Recognizing when your loved one requires specialized care takes empathy, observation, and courage. Subtle changes accumulate into serious concerns that families cannot manage alone. Seeking dementia care provides the peace of mind that daily needs are met with expertise and kindness. More importantly, it allows families to shift their focus from fear to love; spending quality time together while trusted professionals ensure safety, stability, and dignity every day.
Health
5 Ways to Safely Introduce Probiotics to Your Dog

A healthy gut supports a happy life for every pet. Good bacteria help maintain balance within the digestive tract and boost the immune system. Many owners seek natural methods to improve the health of their furry friends. Daily diet choices impact the way a dog feels and acts each day.
Probiotics offer a simple path toward better gut health for pets. These supplements provide live cultures that aid in the breakdown of food. Optimal digestion ensures that a pet absorbs all necessary nutrients from their meals. Many experts recommend canine probiotics to maintain a stable internal environment. This article outlines specific steps to start this health journey safely.
1. Small Portions Support Digestive Balance
New supplements require a slow approach to prevent digestive upset. A sudden change in diet often causes discomfort for a sensitive stomach. Small amounts allow the body to adjust to the new bacterial strains. Probiotics work best when the system accepts them without any sudden stress or shock.
Consistency matters more than a large initial dose for long-term success. Add a tiny pinch of the supplement to the regular morning meal. Watch the pet for any signs of change in mood or appetite. This slow process builds a strong foundation for future health benefits and wellness.
2. Select Specific Strains for Dogs
Different bacterial strains serve various purposes within the animal body. Research shows that certain microbes thrive specifically in the digestive tract of a pet. High-quality products contain stable cultures that survive the journey through the stomach. These specific organisms target the unique needs of a dog’s complex internal system.
Beneficial microbes promote a balanced environment for better health and comfort. Every pet requires a unique blend of cultures to support their daily energy. Experts suggest formulas that focus on the natural flora found in healthy animals. A targeted approach ensures the pet receives the most effective support for their gut.
3. Mix Probiotics with Regular Meals
Palatability plays a huge role in the success of a new supplement. Most pets accept powders or liquids when mixed thoroughly into wet food. The scent of the meal masks the presence of the new addition. This method ensures the pet consumes the entire dose without any struggle or fuss.
- Use a spoon to stir the pet supplement into a bowl of moist kibble.
- Add a splash of water or broth to create a tasty gravy.
- Check that the food stays at room temperature to protect live cultures.
- Offer the meal at the same time every day for a routine.
4. Probiotic Selection Matter
Manufacturers offer various formats to suit the preferences of different pets. Some dogs enjoy soft chews that taste like a favorite treat or snack. Powders provide a versatile option for owners who prefer to measure exact amounts. The right choice depends on the habits and tastes of the individual animal.
- Soft Chews: These treats provide a convenient way to deliver health benefits without a mess. Pets often view these as a reward rather than a medicinal supplement.
- Encapsulated Powders: Capsules protect the live bacteria from light and moisture until the time of use. Owners can open the shell to sprinkle the contents over a meal.
- Liquid Supplements: Liquids offer a fast way to mix microbes into a water bowl or food. This form works well for pets that refuse to eat solid treats.
- Shelf Stable Packs: Individual packets maintain the freshness and potency of each dose for a long time. These remain portable and easy to use during travel or outdoor trips.
- Freeze-Dried Options: This format preserves the integrity of the bacteria through a gentle cold process. It offers a long shelf life while maintaining biological activity.
5. Monitor Daily Progress and Health
Observation remains a vital part of the introduction of any new supplement. Keep a simple log of the pet’s energy levels and digestive habits. Most animals show positive signs of improvement within a few weeks of consistent use. Proper canine probiotics lead to a more vibrant and active lifestyle for the pet.
Patience ensures that the beneficial bacteria have time to colonize the gut. Do not rush the process or increase the dose too quickly. Stick to the plan and watch for a shiny coat and bright eyes. A steady approach leads to the best results for a happy and healthy dog.
Safe introduction of beneficial microbes enhances the life of a pet. Follow these steps to ensure a smooth transition to better gut health. Consistent care and the right bacterial strains make a significant difference in daily comfort. Consider a fiber-rich diet alongside these supplements to provide food for the good bacteria. This holistic strategy creates a robust internal system that supports the animal for many years. Always prioritize high-quality sources to give a pet the best possible support for a long and joyful life.
Health
Laguna Beach Drug Rehab: Getting Better from Addiction

Many people don’t realize how important location is when choosing a place for addiction treatment. Laguna Beach drug rehab centers are well-known for combining high-quality medical care with one of California’s most peaceful natural settings. Located along the Pacific coast, these rehabs offer a unique recovery experience that supports both physical detox and emotional renewal.
Laguna Beach has become a popular destination for individuals seeking meaningful and lasting recovery from drug and alcohol addiction due to its combination of professional treatment and peaceful surroundings.
Why Is Laguna Beach The Best Place To Get Over an Addiction?
People know Laguna Beach for its calm coves, ocean breezes, and laid-back, artistic culture. This setting can help people in rehab manage stress and anxiety, two major factors that often contribute to substance use and relapse.
Laguna Beach is different from busy cities because it feels private and calm. A lot of people choose Laguna Beach drug rehab programs because they let them get away from daily triggers while still getting the best medical and therapeutic care. The beach setting naturally promotes thinking, being present, and emotional balance during treatment.
What Makes Drug Rehab Programs In Laguna Beach Different?
Many Laguna Beach drug rehab centers focus on giving each patient very personalized care. With fewer clients per staff member, treatment teams can create recovery plans tailored to each individual rather than relying on rigid, one-size-fits-all programs.
Most of the time, these rehabs focus on:
- Privacy and confidentiality
- Timelines for treatment that are made just for you
- Mental health care that works together
- A strong focus on healing emotionally
A lot of programs are made to feel less like a hospital and more like a home, which helps clients feel safe, respected, and supported as they recover.
Different Levels of Care Available At Laguna Beach Drug Rehabs
Most drug rehab centers in Laguna Beach offer a full range of care, so you can get help at every step of your recovery.
Medical detox
Detox is often the first step in getting better. Healthcare professionals keep an eye on withdrawal symptoms and make sure that people are comfortable and safe during medical detox programs in Laguna Beach. This step gets the body and mind ready for more in-depth therapy.
Drug Rehab at Home
Many Laguna Beach programs focus on residential or inpatient rehab. Clients stay on-site in a structured, supportive environment that includes daily therapy sessions, wellness activities, and medical oversight. This immersive method works best for people with moderate to severe substance use disorders.
Partial hospitalization and outpatient care
Many Laguna Beach drug rehabs offer partial hospitalization (PHP) and intensive outpatient programs (IOP) for people who are leaving residential treatment or who need more flexibility. These options allow clients to receive regular therapy while gradually returning to daily responsibilities.
Therapeutic Methods Used In Laguna Beach Drug Rehab
True recovery involves more than stopping substance use; it requires understanding the underlying causes of addiction. Laguna Beach drug rehab centers use a mix of evidence-based therapies, experiential therapies, and holistic therapies.
Some common types of therapy are:
- Cognitive Behavioral Therapy (CBT)
- One-on-one therapy
- Peer support and group therapy
- Therapy sessions for families
Many Laguna Beach rehabs also offer trauma-focused therapy because they know that unresolved emotional pain can lead to drug and alcohol use. Directly dealing with trauma can make recovery much better.
Integrating Holistic Healing And Wellness
The focus on whole-person wellness is one thing that makes Laguna Beach drug rehab stand out. Treatment programs often go beyond regular therapy to include things that help with mental clarity and physical health.
These could be:
- Meditation and mindfulness practices
- Yoga and breathing exercises
- Advice on nutrition
- Therapy based on nature and walks on the beach
The ocean itself helps people heal. Being near water has been shown to lower stress, improve mood, and help with emotional regulation, all of which are important for early recovery.
Laguna Beach Dual Diagnosis Treatment
A lot of people who go to rehab have both an addiction and a mental health problem like anxiety, depression, or PTSD. Laguna Beach drug rehab centers often focus on dual diagnosis treatment, which means that both conditions are treated at the same time instead of one at a time.
This integrated approach reduces the risk of relapse and helps clients develop healthier coping strategies for stress.. Treating both mental health and substance abuse at the same time makes long-term recovery more likely.
Aftercare And Ongoing Support After Rehab
To stay sober after treatment, you need a strong aftercare plan. Laguna Beach drug rehabs put a lot of effort into getting their clients ready for life after the program.
Some aftercare services are:
- Therapy on an ongoing basis
- Referrals for sober living
- Relapse prevention planning
- Programs for alumni and peers to help each other
These tools help people stay connected, responsible, and supported as they go back to their normal lives.
How To Pick The Best Laguna Beach Drug Rehab?
Choosing the right rehab is a personal choice that should fit your needs, goals, and values. When looking into drug rehab options in Laguna Beach, you should look for facilities that are licensed, have experienced clinical staff, and are open about their treatment methods.
Many centers offer private consultations to talk about your history of drug use, mental health needs, and lifestyle choices. A program that fits well can make a big difference in how well someone recovers.
Going Toward a Healthier Future
Laguna Beach drug rehab centers do more than just help people get better; they also give them a place to start over, heal, and rebuild. With professional care, personalized therapy, and a peaceful coastal setting, getting better is a real and long-term goal.
Laguna Beach offers an ideal environment for individuals who want to start over, step away from daily chaos, and focus on genuine healing. It supports healing at every level. Addiction may have shaped some of the past, but it doesn’t have to shape the future if you get the right help.
-

 Finance3 years ago
Finance3 years agoProfitable Intraday Trading Advice For Novices
-

 Gaming2 years ago
Gaming2 years agoPixel Speedrun Unblocked Games 66
-

 Gaming3 years ago
Gaming3 years agoSubway Surfers Unblocked | Subway Surfers Unblocked 66
-

 Internet3 years ago
Internet3 years agoWelcome to banghechoigame.vn – Your One-Stop Destination for Online Gaming Fun!
-

 Gaming3 years ago
Gaming3 years agoMinecraft Unblocked Games 66 | Unblocked Games Minecraft
-

 Gaming3 years ago
Gaming3 years agoGoogle Baseball Unblocked | Google Doodle Baseball Unblocked 66
-

 Internet3 years ago
Internet3 years agoPremium Games Unblocked: Unleash Your Gaming Potential
-

 Gaming3 years ago
Gaming3 years agoTunnel Rush Unblocked | Tunnel Rush Unblocked 66